A good method to measure heart rate (HR) using sensor data
I will present here a good method to measure heart rate (HR) using sensor data and investigate the effect of feedback loops on HR rhythms.
I will show you answers to these specific questions:
- What is the best way to calculate resting baseline heart rate (HR) using ECG sensor data and RR intervals?
- What is the best way to calculate movement/exercise heart rate (HR)?
- What is the best way to calculate instantaneous heart rate (HR) biofeedback?
Let's start.
1. What is the best way to calculate resting baseline heart rate (HR) using ECG sensor data and RR intervals?
The research gives the motivation to use time-series statistics to partition and decompose the beat-to-beat (RR) heart rate signal into periodic components representing plausible neurophysiological feedback loops on the cardiac pacemaker [1]. The research also proposes a two-case scenario, depending on if we can deduce the breathing (respiratory) cycle or not [2].
1.1 If we are unable to deduce the breathing (respiratory) cycle
Assuming we are measuring healthy individuals, we can use the mean HR measure for the resting baselines recording. That said, we need to carefully remove artifacts in the RR intervals signal.
The research states that the mean HR measure is derived from direct measurements of RR intervals or instantaneous heart rate [3]. The research also (questionably) states that the mean HR measure is the average HR during 5 minutes, and the normal expected values of mean HR are between 60-90 bpm [4].
1.1.1 What causes lower HR - below 50 bpm (Bradycardia)
- Physically healthy individuals who exercise hard and regularly
- Pharmaceutical drug side effects
- Functional/anatomical heart problem (Heart failure/Heart arrest)
- Hypothyroid, Hypothermia
1.1.2 What causes higher HR - over 100 bpm (Tachycardia)
- Normal response to the exercise and acute emotional change(anxious and frightened)
- Effects of caffeine, alcohol, nicotine, and other drugs
- Weakened general health, Lack of sleep
- Stress and anxiety
- Anemia
- Hyperthyroid, Dehydration
- ANS dysregulation
- Functional/anatomical heart problem
Note that the attention is necessary if:
- there’s long term tachycardia without heart rate deceleration
- an experience of syncope, dizziness, chest pain, weight loss, or headache
1.2 Heart period RR vs. heart rate HR
The authors stress that while the function relating vagal activation to heart period RR is relatively linear over normal operation ranges, for heart rate HR is hyperbolic and so a non-linear transformation of RR intervals [5]. Even though relationships between RSA or other parasympathetic-based rhythms should be independent of timing (chronotopic) state, this does not hold for heart rate. The sympathetic relationship is somewhat more complex as it is non-linear for both Heart period RR and heart rate HR, but it still behaves linearly over normal operating ranges for heart periods RR. The dynamic range of parasympathetic is considerably greater than sympathetic, and vagal control can introduce baseline dependency in sympathetic estimates if expressed through heart rate.
Therefore, to avoid loss of parasympathetic HF resolution, heart rate should be derived on a beat-by-beat basis and a time series should be derived.
- Heart rate variability actually concerns measures derived from either heart rate HR or heart period data RR
- Heart period variability should be used only when the analysis is based on RR interval data
1.3 Direction of beat-to-beat heart rate changes
Another interesting HR parameter is the direction of beat-to-beat heart rate changes. The direction can accelerate or decelerate. In Classical Conditioning, in Phasic Heart Rate Responses the acceleration in infants may reflect autonomic arousal triggered by stimuli. The cardiac deceleration in adults may indicate cognitive awareness that reward will follow the stimuli, leading to an orienting response. Nevertheless, slow heart rate tends to increase after Bainbridge reflex (arterial baroreflex), while rapid heart rates tend to decrease. This is the mechanism in effect on RSA.
We can calculate 'heart index' (iH) by dividing each target RR interval by the pre-trial RR interval + the target RR interval, i.e., iH = RR(n)/(RR(pre) + RR(n))
An iH value >0.5 would indicate cardiac deceleration (larger interval length), while iH value smaller than 0.5 would indicate cardiac acceleration (smaller interval length). The absolute values of iH indicated the magnitude of the phasic heart rate changes [6].
1.4 Breathing rate experiment
Increasing breathing depth raises HR Max − HR Min value (increasing HR variance), but it does not reduce time-domain, frequency-domain, or non-linear HRV measures parameters (doesn't change the mean HR). A fun experiment is to make a recording with paced breathing of around 7 bpm and another with 14 bpm and to observe the change in HR variance and stable mean HR between the two recordings.
| RSA (7 Hz) | non-RSA (14 Hz) | |
|---|---|---|
| HR | 69.45 | 72.13 |
| RMSSD | 85.90 | 45.35 |
| LF | 4935.27 | 1085.98 |
| HF | 815.67 | 493.36 |

Difference between top image RSA (7 Hz) vs. bottom image non-RSA (14 Hz). They both resulted in similar HR values, but the difference is obvious in RMSSD HRV values.
Judging from the HR results we could say that these two case studies are very similar to each other since they resulted in similar HR values. But only after we observe the RMSSD HRV values we can observe what effect breathing has on our heart, using the mechanisms explained. Figures also demonstrate the difference between these two cases.
All of this information can be found on the graph the in Brainjam app, at one glance. With HR illustrated as the red line, and HRV RMSSD illustrated as bars (it even shows the development of HRV overtime during the duration of recording).
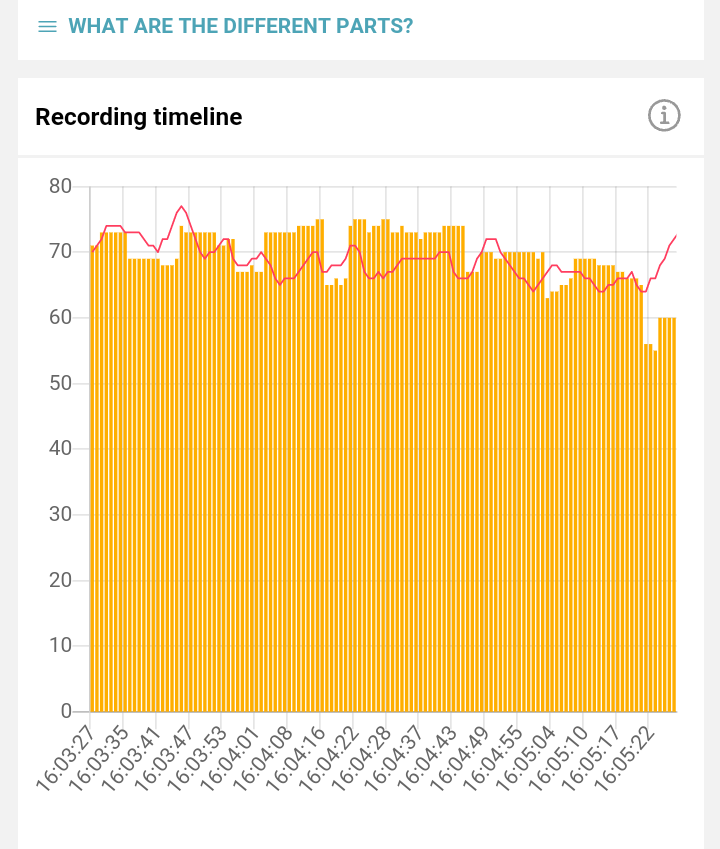
Top image RSA (7 Hz).
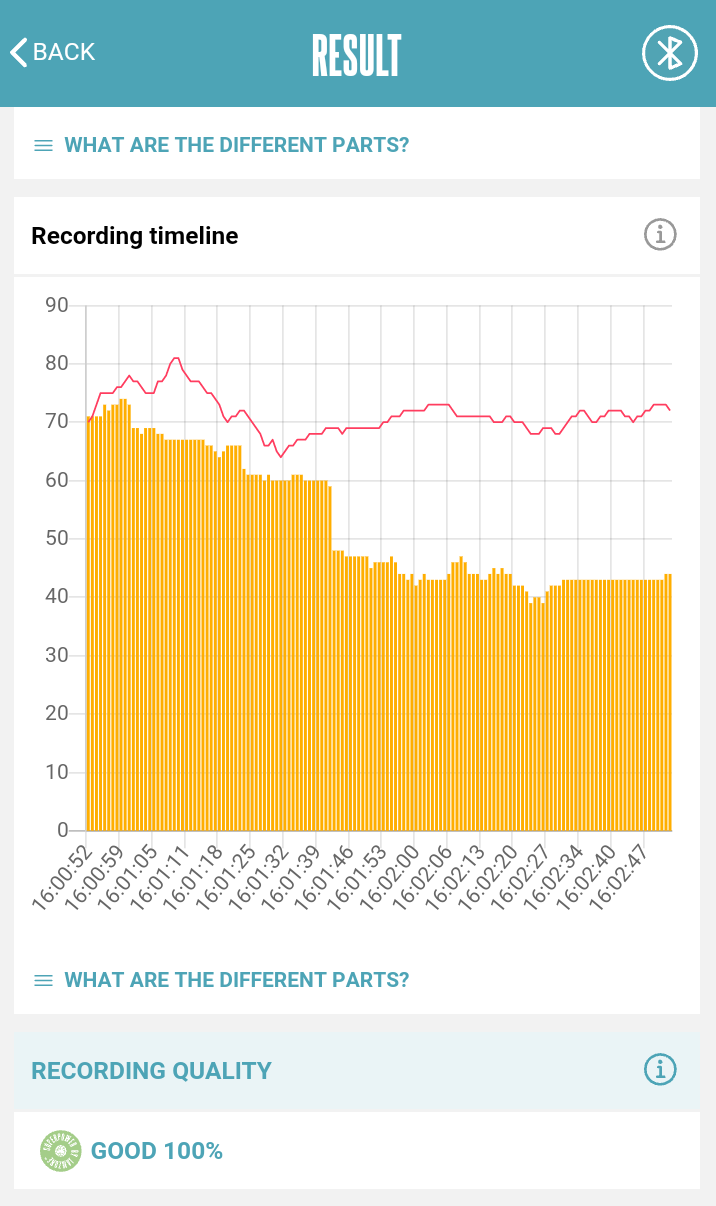
Bottom image non-RSA (14 Hz). They both resulted in similar HR values, but the difference is obvious in RMSSD HRV values.
1.5 Proposal for a beat-by-beat HR calculation method
I will demonstrate here the preferred beat-by-beat HR calculation vs. using the average RR interval in some period. I will give two examples of heart rate HR calculation generated with a normal random number generator (with and without prominent outliers).
| HR calculation | Beat-by-beat | Average RR interval | True HR |
|---|---|---|---|
| wout/outliers | 60.396 | 59.932 | 60 |
| w/outliers | 63.965 | 60.585 | 60 |
| control | 101.724 | 100.966 | 102 |
As you can see in the table above, both methods give similar results with beat-by-beat HR calculation being more precise under control conditions. Nevertheless, the presence of outliers is the biggest problem of HR calculation, and this demonstrates that we need to always clean outliers before the analysis.
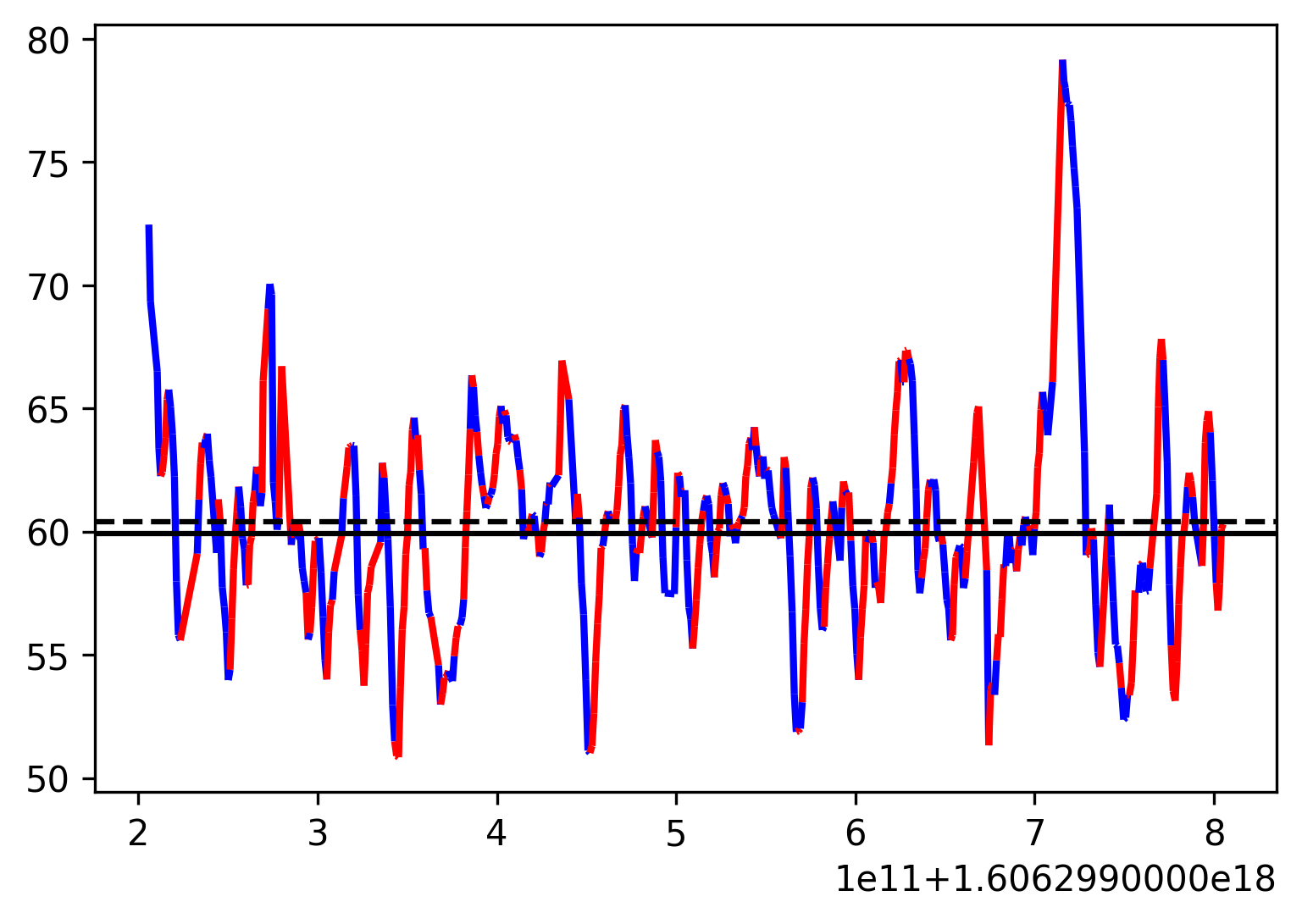
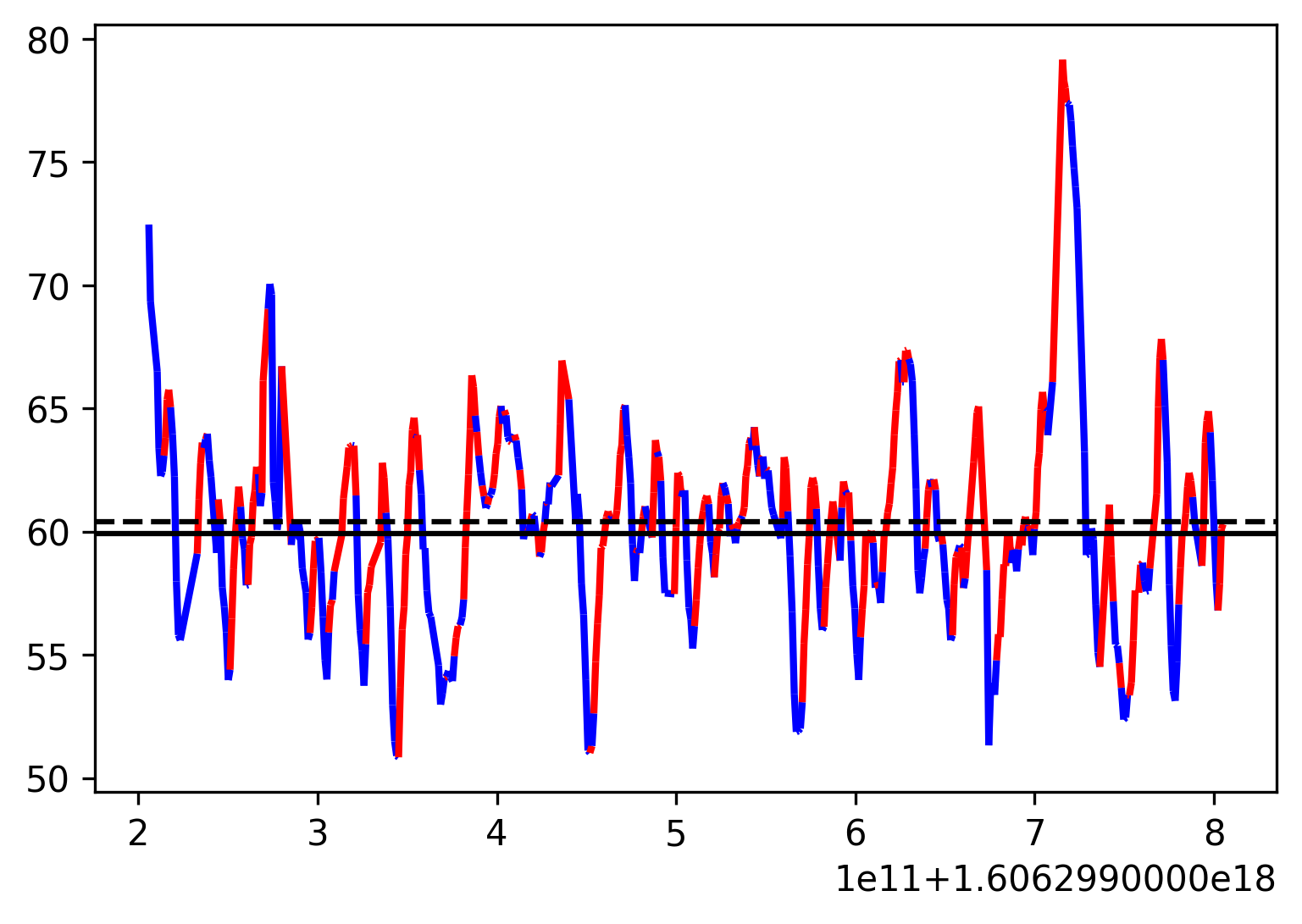
Let's plot the above-mentioned examples with outliers removed.

Top image is the control condition recording, and the bottom image is the regular recording without outliers (removed). The dashed line is the Beat-by-beat method and the solid line is the Average RR interval method.
1.6 If we are able to deduce the breathing (respiratory) cycle
Peak-to-valley statistical methods
The most optimal measure is the average difference between the highest and lowest HRs during each respiratory cycle (HR Max − HR Min). The HR Max − HR Min measure is especially sensitive to the effects of breathing rate, this is why we need breathing cycle information to be able to use it correctly.
The authors give information that this specific time-domain short-term variability analysis method is useful to identify respiratory frequency oscillations (RSA) selectively from other components [7]. It is defined as a breath-by-breath peak-to-valley measure of heart rate fluctuations. The statistics represent the difference between the longest and the shortest heart period within the respiratory cycle. Basically, it is the maximum heart period associated with inspiration and the minimum heart period associated with the expiration for each respiratory cycle in the recording. This method gives a simple range of statistics that achieves respiratory frequency selectivity by directly registering heart rate changes to the ongoing respiratory rhythm.
HR Max − HR Min measure is largely independent of vagus nerve traffic, which adds to its stability. Therefore, it reflects coherent breathing a.k.a. respiratory sinus arrhythmia (RSA) instead of directly indexing vagal tone. The mechanism of its independence is the following. Slower breathing rates can produce higher RSA amplitudes that are not communicated by changes in vagus nerve traffic. This is because longer exhalations allow greater acetylcholine metabolism, which slows down the SA node depolarization and discharge rhythm.
The sinoatrial node (SA) is the endpoint of the nervous system at the heart and therefore influences the rhythm of the heart.Successive RR intervals are a series of data points spaced unevenly in time, as heartbeats happen. Time-series analysis assumes that the data is sampled at equal time intervals. Therefore, the successive RR series doesn't qualify for time-series analysis. (interpolated and evenly resampled to avoid distortions in the spectra). Interpolation may alter the final spectrum, especially when ectopic beats occur and a broadband noise contaminates the spectrum. This is why the ectopic beats are necessary to clean from the analyzed signal.
The Lomb method (generalized Lomb method to estimate transforms of unevenly sampled data) for spectral powers estimation is based on the minimization of the squared differences between the basis function of the transform and the signal under study. When the signal is accessible only at unevenly spaced intervals, the Lomb method proposes to estimate the Fourier spectra of a signal by adjusting the model in such a way that the variance of estimation is minimized.
The Lomb method is used to analyze randomly sampled data avoiding spectrum distortion since it doesn't need interpolation and doesn't suffer from the above-mentioned problem with ectopic beats. Nevertheless, breathing oscillations introduce non-linear and non-stationary rhythmic patterns in the ECG data and it can influence the performances of the Lomb method. Using wavelet transformation we might extract the components which might be speculatively associated with breathing.
The empirical mode decomposition EMF (wavelet transformation) decomposes a time series into components with well-defined frequency by empirically identifying the physical time scales intrinsic to the data. Each component oscillatory mode extracted is named intrinsic mode function (IMF). After the method, we have a collection of IMFs in the descending order of frequencies and a residual signal. We can reconstruct the original signal using the mathematical relationship of summing all the IMFs and adding the residual signal. Usually, the first such IMF associated with the locally highest frequency is associated with breathing oscillation.
1.6.1 Steps to obtain HR cleaned from the breathing rhythms
- Window the data in 1-min windows
- Transform the signal to zero-mean and detrend
- Obtain the IMF associated with breathing oscillation
- Clean the instantaneous heart rate signal by subtracting the obtained IMF from the original signal
- Calculate the Lomb method from such cleaned instantaneous heart rate signal
2. What is the best way to calculate movement/exercise heart rate (HR)?
While performing exercises with vigorous movements, it is beneficial to combine the movement sensor together with the ECG HR sensor to obtain more accurate results. Because of the low accuracy of traditional heart rate acceleration motion wireless sensors in athlete heart rate recognition and motion state recognition in competitive sports, this paper proposes an athlete heart rate recognition algorithm based on acceleration signal, which fully extracts the frequency-domain, time-domain, and time-frequency features of athlete acceleration signal to realize the recognition of motion state; the accurate detection of athletes’ heart rate is realized by power spectrum cancellation technology [8] [9].
3. What is the best way to calculate instantaneous heart rate (HR) biofeedback?
We can also take the second example and plot the heart rate index in red/blue color where heart rate increased/decreased - window 5 sec. We notice great variability in individual heartbeats that the average of 5 sec might not be able to collect.
We can also take the second example and plot the heart rate index in red/blue color where heart rate increased/decreased - window 10 sec. We still notice variability in individual heartbeats, but we gained stability in direction of individual heartbeats. Therefore, 10 seconds might be a better window to calculate the HR average that can collect most of the individual heart-beat variability.
Conclusion
Regarding the resting baseline heart rate (HR) using ECG sensor data and RR intervals. Taking all this information into consideration, depending on if we are able to deduce the breathing (respiratory) cycle.
- If we are unable to deduce the breathing (respiratory) cycle
- Resting baseline recording - a 10-sec sample recording is sufficient to measure mean HR, while 1 min sample recording is sufficient to measure other HRV parameters, i.e., SDNN and RMSSD (but those are altogether another story)
- If we are able to deduce the breathing (respiratory) cycle
- Resting baseline recording - at least a 2-min sample recording is required to measure HR Max − HR Min.
Regarding the movement/exercise heart rate (HR), it is beneficial to combine the movement sensor together with the ECG HR sensor to obtain more accurate results.
Regarding the instantaneous heart rate (HR) biofeedback, a 10-sec sample recording is sufficient to measure mean HR.
